The Fraser Eye Care Center Doctors have either authored or reviewed and approved this content.
The eye doctors at Fraser Eye Care in Detroit, Michigan have experience in treating a range of retinal conditions and diseases, including macular degeneration. Through early diagnosis and prompt treatment of macular degeneration, we can help preserve patient’s eye health and vision.
The retina is located at the back of the eye: it is a layer of cells that sends light to the optic nerve, where it is converted into images. Age-related macular degeneration (AMD) is an eye condition that causes degeneration of the macula, the area of the retina responsible for central vision. This causes slow central vision loss. Peripheral (side) vision is not affected by macular degeneration.1
AMD is a common condition, and is the leading cause of blindness in people over the age of 50, according to the American Academy of Ophthalmology.2
There are two types of macular degeneration: dry macular degeneration and wet macular degeneration.
The dry form of macular degeneration, (non-neovascular or atrophic macular degeneration) is the most common form of this condition by far, affecting up to 90% of patients. Dry macular degeneration is caused by drusen, which are protein deposits that can form under the macula. Over time, this can cause the macula to become thinner and more dry. Patients with dry AMD experience gradual vision loss that rarely results in total blindness. Rarely, dry macular degeneration can progress to wet macular degeneration.
Wet macular degeneration (neovascular or exudative macular degeneration is the result of the formation of abnormal blood vessels under the macula and retina. In wet AMD, the abnormal blood vessels exude blood and fluid, causing the macula to bulge. Loss of central vision in patients with wet AMD can be sudden and complete.3
When AMD is in its early stages, patients may not encounter any vision problems or other symptoms. As dry macular degeneration progresses, patients may begin to notice:
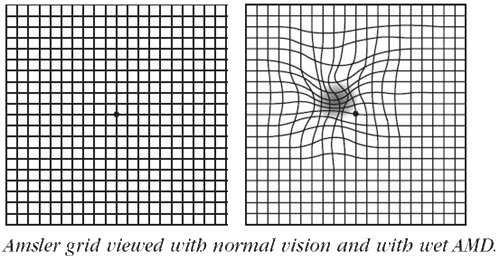
If a patient has wet AMD, visual distortion may include straight lines that appear wavy and increasing blind spots. Vision loss from wet macular degeneration can occur very suddenly, even over the course of days.
Age related macular degeneration is a leading cause of vision loss in people over the age of 50. While there is no cure for AMD, it is possible to slow its progression, which is why it is so important to have regular eye exams. If signs of macular degeneration are identified early, prompt treatment can slow or even prevent vision loss.
The first step an ophthalmologist will perform to diagnose age-related macular degeneration is a dilated eye exam. Additional tests that will lead to a definitive diagnosis include:
Age-related macular degeneration is progressive, and the stages of AMD are classified by signs identified by an eye doctor as well as the patient’s symptoms.
Early stage macular degeneration is characterized by a higher-than-usual presence of drusen, or yellow deposits, under the retina. Most patients with early stage AMD do not experience symptoms.
In intermediate stage AMD, large drusen and changes in the pigment of the retina can be observed by an ophthalmologist. Visual impairment is usually not present during intermediate stage macular degeneration, though patients may notice small gaps in their vision.
When a patient is in late stage macular degeneration, severe retinal damage has resulted in severe vision loss. At this stage of AMD, patients may notice that straight lines appear wavy.
There is no cure for AMD, but it may be possible to slow its progression and reduce or prevent vision loss.
The National Eye Institute states that patients with wet AMD may be able to reduce further vision loss by:
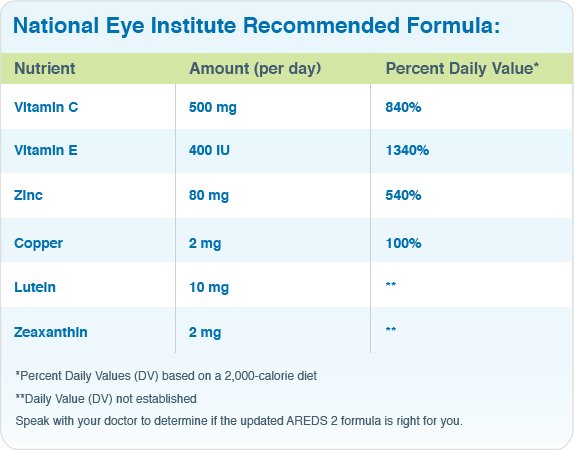
It is now believed that a key to managing age-related macular degeneration is a system of vitamin and mineral supplementation known as AREDS or AREDS2. Studies conducted by the National Institute of Health called the Age-Related Eye Disease Study (AREDS, followed by AREDS2) investigated whether daily use of certain vitamins and/or minerals may help delay the progression of AMD.
The formula recommended by the National Eye Institute includes high levels of antioxidants and zinc, which may help reduce the risk of advanced AMD vision loss by up to 25%. These supplements do not sufficiently benefit patients in early or intermediate stage dry macular degeneration, nor do they restore vision already lost to AMD.5
Can macular degeneration be prevented?
What are the risk factors for macular degeneration?
How can I improve my vision with macular degeneration?
For more information on macular degeneration and to schedule an examination by an experienced ophthalmologist, please contact us. We proudly serve patients from throughout the Detroit, Michigan area.
1 Cleveland Clinic. Retina. Available: https://my.clevelandclinic.org/health/body/22694-retina-eye#:~:text=The%20retina%20is%20made%20of,field%20(your%20peripheral%20vision). Accessed September 13, 2022.
2 American Academy of Ophthalmology. What is Macular Degeneration? Available: https://www.aao.org/eye-health/diseases/amd-macular-degeneration. Accessed September 13, 2022.
3 Cleveland Clinic. Age-Related Macular Degeneration. Available: https://my.clevelandclinic.org/health/diseases/15246-age-related-macular-degeneration. Accessed September 13, 2022.
4 American Academy of Ophthalmology. How is AMD Diagnosed and Treated? Available: https://www.aao.org/eye-health/diseases/amd-treatment. Accessed September 13, 2022.
5 National Eye Institute. Age-Related Macular Degeneration. Available: https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration. Accessed September 13, 2022.
6 BrightFocus Foundation. Age-Related Macular Degeneration: Facts & Figures. Available: https://www.brightfocus.org/macular/article/age-related-macular-facts-figures. Accessed September 13, 2022.
The Fraser Eye Care Center Doctors have either authored or reviewed and approved this content.